Disclaimer Before You Start Reading
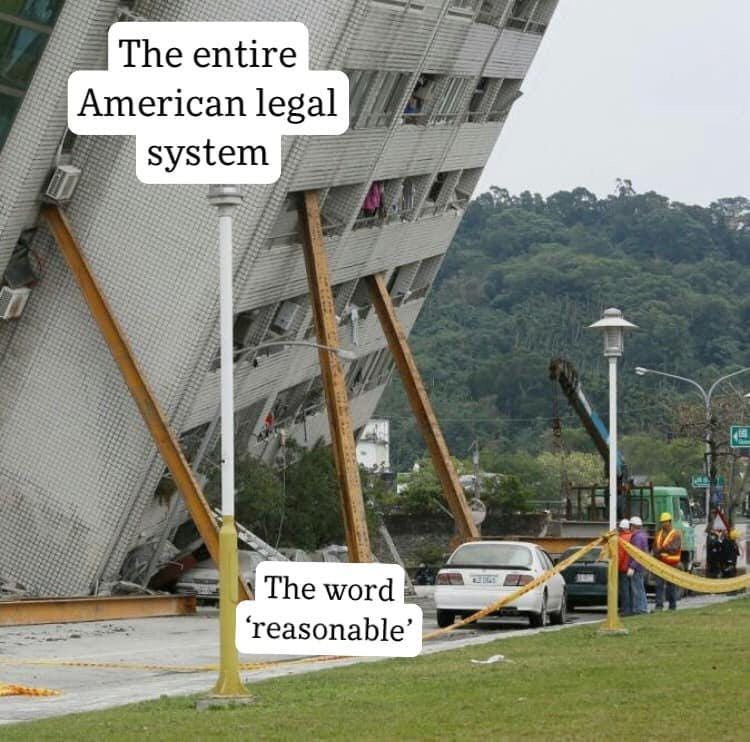
I am not a lawyer. I have no formal legal training. I listen to Supreme Court arguments, the Advisory Opinions podcast, and have gotten semi-familiar with Massachusetts civil commitment and healthcare proxy laws as a hobby. Please do not read this and assume that my interpretations are correct and then make legal decisions based off of them. My general understanding of the law can be summed up by this meme:1
When I quote the text of various statutes and their chapters, articles, subsections, etc. I will try and make it clear which statute I am referring to so you can read the primary text itself. I will also be omitting parts of the text that are not useful to the conversation; things like “an advanced practice registered nurse authorized to practice as such under regulations promulgated pursuant to section 80B of said chapter 112.”
Also I am avoiding anything that has to do with minors because I’m not doing CAP and never will.
To some degree, this piece is to help me start understanding the intricacies of North Carolina’s mental health laws,2 which I feel an obligation to understand beyond what will be filtered through to me in mandatory training modules. I think it will also be interesting to see how much I was able to understand correctly from my own reading of the statute, and what I will inevitably be wrong about once I’m in practice.
If you’re a practicing psychiatrist I hope that you will come to appreciate the utility of reading and attempting to understand the nuance of commitment laws. We are one of a very small group of private citizens who are regularly imprison people against their will,34 and I think that means we should make a serious attempt to (1) understand what the law actually says; (2) try and get a loose grasp on what the law intends; (3) use this information to act within the bounds of our authority and to understand when we are starting to ignore our best understanding of the intent of the law (and then not ignore it).
If you’re not a psychiatrist, I hope that this will help to give you a better understanding of just how much leeway the law gives to physicians as part of this process and how this allows individual psychiatrists to make such different decisions despite operating under the same laws. There is a lot of subjectivity in interpreting these laws; I’ve found that even case-law5 that is on-point can be contradictory and subjective.
Speaking of the law, I will mostly be looking at North Carolina General Statute, Chapter 122C. For those of you who want to follow along at home, I’m going to spend most of my time looking at the various subsections of Article 5 - Procedure for Admission and Discharge of Clients.
Define Your Terms
There’s something very important that needs to be addressed first. Something that didn’t even occur to me to ask when I started out in training. What does “mental illness” mean when we talk about the law? How does the law define it? How do we know?
Fortunately, there are these neat little sections at the beginning of lots of laws (statutes? whatever) that usually define high-level terms. Unfortunately, lawmakers sometimes don’t include definitions for terms that are really important and/or don’t tell you where to look to find the definition.
A great example of this can be found in Massachusetts General Law Part I, Title XVII, Chapter 123, Section 12 which contains the section under which we involuntarily commit people to the hospital for “mental illness:”
A physician… who, after examining a person, has reason to believe that failure to hospitalize such person would create a likelihood of serious harm by reason of mental illness may restrain or authorize the restraint of such person and apply for the hospitalization of such person for a 3-day period at a public facility or at a private facility authorized for such purposes by the department.
You’ll notice that this part of the text never says what “mental illness” actually means, and nowhere else in Section 12 will you find a definition. No worries, we should be able to go look at Chapter 123, Section 1 which contains the definitions used in the chapter:

Usually I try to be charitable about this sort of thing… but… uh… wow.
Turns out that there is a definition of mental illness that is not a law, but exists as part of a regulation promulgated by the MA Department of Mental Health (DMH) - 104 CMR, § 27.05 - General Admission Procedures. Is this the definition of “mental illness” that I’m supposed to be referencing? I think so, based on what’s on the physical Section 12 forms that the MA government puts on its website. This defines “mental illness” as:
…a substantial disorder of thought, mood, perception, orientation, or memory which grossly impairs judgment, behavior, capacity to recognize reality or ability to meet the ordinary demands of life, BUT shall not include intellectual or developmental disabilities, autism spectrum disorder, traumatic brain injury or psychiatric or behavioral disorders or symptoms due to another medical condition as provided in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), 5th edition published by the American Psychiatric Association, OR except as provided in 104 CMR 27.18, alcohol and substance use disorders; provided however, that the presence of such conditions co-occurring with a mental illness shall not disqualify a person who otherwise meets the criteria for admission to a mental health facility.
That is some pretty vague language DMH. What does “substantial” mean? What does “grossly impairs” mean? Why did you use a run-on sentence instead of a numbered list after the first “BUT” that would’ve clarified things greatly?
If you thought that definition was broad, North Carolina would like to show you what the word vague really means when it defines “mental illness”:
When applied to an adult, an illness which so lessens the capacity of the individual to use self-control, judgment, and discretion in the conduct of the individual's affairs and social relations as to make it necessary or advisable for the individual to be under treatment, care, supervision, guidance, or control.
As a psychiatrist, this definition is great for me because approximately 100% of people that I think should be hospitalized for their psychiatric problems have an illness that “lessens their capacity to use self-control, judgement, and discretion” due to which it would be “advisable” for that individual to be “under treatment.” It is, however, a definition so vague that it sweeps in a lot of what I think of as traditionally “neurological” diseases6 like dementia and delirium.
Speaking of the word ‘illness’… what exactly does that mean?
Er, let’s move on.
I’m sure many of you reading these statutes for the first time looked at these definitions and thought — like I did — that it was ridiculous how broad they were.
Surely, surely! there has to be a better, narrower definition, somewhere. My first thought was: Why not just use diagnoses in the DSM-57 as our source of definitions? Maybe exclude the “unspecified” diagnoses to limit abuse? That sounds… pretty good?
The more I thought about that, the more tepid my enthusiasm became. First, the DSM includes more diagnoses than you think, many of which I’m not sure I’d like to sweep in (e.g. dementia, intellectual disability, personality disorders). I suppose we could exclude specific items, but I’m not sure I really trust legislators to do that.
There is also the distorting effect that being used as a source of law would have on the DSM itself. The DSM is already filled with various diagnoses that are kept around — not because we think they are valid or useful constructs — but because of psychiatric politicking (I’m looking at you personality disorders8). Imagine how much less useful and more contentious the DSM would get if people could only be hospitalized for illnesses explicitly defined within it!
On the other hand, I don’t want to be hamstrung by overly narrow definitions written by legislators who only have a surface-level understanding of what the facts on the ground are. Sometimes, all I know is that the person is obviously psychotic, but I can’t get any more information out of them to form a more complete diagnosis because they feel that it is really important that I know that even though their skin looks black, they are actually a white person, but their neighbor’s A/C has been darkening their skin by delivering electric shocks through the wall. Also they would love to give me contact information for their mother who knows them very well, but it turns out that their neighbor has been spying on them via other electronics so they threw their phone into the Charles a week ago.
Is this drug induced? A psychotic depression? A psychotic mania? Just good ‘ole schizophrenia? This is usually not something I can determine based on speaking with a patient for an hour or so, especially if there’s no collateral.
My present conclusion is that this problem is not solvable without some sort of tradeoff9. I don’t think there is a good way to write a law that gives us a large amount of flexibility without opening an avenue for a lot of abuses of civil liberties.
Right now, it seems like most laws are written in a way that says to people like me, “Hey, we don’t want to hamstring you too much, so we’re going to give you very broad definitions and trust you to interpret them responsibly.” We should be appreciative of the leeway that society has granted us and mindful of the fact that it can be taken away if we play too fast and loose with the rules too often.
I emphasize this is because we are incredibly insulated from the social, legal, and financial consequences of involuntarily hospitalizing patients; even if it’s “just” for a 72h initial observation. We don’t risk losing our jobs or being unable to pay rent because we missed 3 days of work. We don’t have to worry about leaving our pets alone without anyone to feed or water them. We don’t have to leave our spouse to figure out who is supposed to watch the kids when they have a work shift. We don’t have to miss our child’s birth, a parent’s funeral, or a friend’s wedding.
Of course — of course — there are times where these are unfortunate, but totally reasonable tradeoffs, for, say, treating someone’s psychotic mania. There are other times where we do it to make ourselves feel better… er, I mean, “just to be safe.” My firm, but gentle, suggestion is that we should try and avoid doing that second thing.
Liability
Ah, liability. Always good to understand how liable am I if I screw this up. Well, § 122C-204 says:
Nothing in this Article relieves from liability in any suit instituted in the courts of this State any individual who unlawfully, maliciously, and corruptly attempts to admit or commit any individual to any facility under this Article.
Ok, so don’t don’t be malicious and corrupt or you don’t get the protections in this Article got it... What sort of protections are we talking about?
§ 122C-210.1 explains:
No facility, person, or entity, [list of lots of specific people/entities] or any other physician or individual who is responsible for the custody, transportation, examination, admission, management, supervision, treatment, or release of a respondent or client AND who is not grossly negligent, is civilly or criminally liable, personally or otherwise, for that person's or entity's actions or omissions arising from these responsibilities or for the actions or omissions of a respondent or client…
That’s a little hard to read, let me try and simplify:
No facility, person, or entity…
who is responsible for the custody, transportation, etc. of a respondent or client, AND who is not grossly negligent,
is civilly or criminally liable, personally or otherwise, for that person's or entity's actions or omissions arising from these responsibilities or for the actions or omissions of a respondent or client…
So basically I can’t be civilly or criminally liable unless I:
Maliciously and corruptly commit someone
You might say to your yourself (like I did) the following: “Ok, well, why bother reading on? As long as I’m not cosplaying Aubrey Levin or Andrei Snezhnevsky and generally try to follow the rules, I should just do what I think is right and not care about the details.”
What I worry about with that thought process is the following: We are rather conditioned in medicine to think of the “right thing” as being more conservative rather than less. I’m willing to bet that the first thought most psychiatrists reading this section had was:
“Well, good, now I don’t have to worry about getting in trouble for hospitalizing someone involuntarily.”
Not so much:
“Well, good, now I don’t have to worry about getting in trouble for not hospitalizing people ‘just to be safe.’”
You know how doctors constantly complain about having to practice “defensive medicine?” Seems like the phrasing in § 122C-210.1 might alleviate some of those worries.
Voluntary Admissions
In the psychiatric world, patients in psychiatric hospitals tend to fall into two categories: Voluntary and Involuntary. The differences between the two are fairly implicit in their naming. However, different states deal with these patients differently in terms of the legal status under which they must present to a hospital and where they are placed once hospitalized.
Some states separate their voluntary and involuntary psychiatric units. On voluntary units, patients are still considered to be hospitalized and in some cases are unlocked (i.e. patients are free to leave and return to the unit). Involuntary units are, as you might have guessed, locked.
Some states — like Pennsylvania — allow for patients to present voluntarily for admission. Other states, like Massachusetts, have a confusing nightmare system where the law only contemplates that someone would be going to an inpatient facility involuntarily and so every patient must be brought to an inpatient unit on an involuntary hold. This requires an attestation from someone11 that the patient is either a danger to themselves or others due to their mental illness. For voluntary patients, this often results in very awkward and legally dubious situations where we have to sign a document attesting that we think that a patient is a danger to themselves/others — even though we do not think that12 — otherwise no inpatient until will take them. Because everyone is “involuntary” on arrival, Massachusetts has no unlocked inpatient units.
Fortunately, North Carolina’s law is less insane (so far) and allows for voluntary admissions to via § 122C-211.
I’ll summarize:
Any individual in need of treatment for mental illness or substance abuse can present for evaluation, as long as they submit a written application for evaluation or admission. Obviously, then an evaluation to determine if they need to be hospitalized has to happen. Interestingly:
Information provided by family members regarding the individual's need for treatment shall be reviewed in the evaluation.
The word “shall” raises a lot of questions here. Which family members? How many? If there are no family members available, but the patient obviously needs to be hospitalized, is the evaluation considered “incomplete” until I can speak to one?13
The person doesn’t have to be accepted if they “[do] not need or cannot benefit from the care,” — if they would benefit from a lower level of care, we’re obligated to refer them to somewhere that can provide them that treatment.
If “medical care is an integral component of the treatment,” the patient needs to be evaluated by a physician within 24h of admission. If medical care is not an an “integral component” then either the patient needs to have a documented medical evaluation within 30 days (before or after) of admission.14 What, exactly does “medical care” mean? I might assume that since I am a MD and psychiatry is a medical specialty, that such a definition would necessarily include psychiatric care and so the exam needs to be done in 24 hours. On the other hand, this entire section of the statute is all about psychiatric care, so the writers must think that there is some type of voluntary psychiatric admission that does not feature medical care as an integral component of the treatment, so maybe they’re talking about the more traditional concept of “medical care” like managing diabetes and hypertension or whatever?
Once accepted to the facility, the patient can request to leave at any time, but can be held for an additional 72h after that request. This seems rather lengthy, but it solves a couple problems:
First, it prevents patients who would otherwise be committed from being discharged over the weekend. Often, weekend shifts are covered by just a couple physicians, who probably don’t know very much about the patient and are unlikely to be able to make an informed decision about whether or not commitment is appropriate. Honestly, I think this is probably why it’s 72h instead of 24h or 48h.
Second, it gives the psychiatrist time to consider whether or not commitment is necessary, consult with the hospital legal team, and put together the documents for commitment if it is. This can usually be done inside of 24h on a weekday.
Third, this big of a window makes it pretty hard for wily patients who know the system to strategically pick a time to submit their request for release. You can imagine a situation in which the hold only lasted 12 hours, in which the patient submits their request at 6pm.
This 72h rule, again, allows me to make my point about the importance of not just attempting to follow the law per se, but the intent behind it.
As written, you can keep any voluntary patient for 72h after they request their discharge. There are no strings attached to this that I can see, unless maybe you are dumb enough to put in writing that you are holding the patient for the full 72h because they pissed you off a little bit yesterday and now they need to sit in their room and think about what they did.
It seems to me that — again — the law is saying “Hey, we know this stuff is difficult and deserves some contemplation, we don’t want people having to figure this stuff out over weekends… here’s 72h to make a decision. We trust you.”
So, again, we should feel at least a little responsibility to minimize the amount of that time that we actually use and prioritize discharging patients who we don’t think meet commitment criteria. We shouldn’t be holding people for an extra 24h because “today was just a really busy day,” or “we only do two discharges a day.”15
Incapable Adults
For this next bit to make sense, we need to make another detour, this time into the land of what North Carolina calls “incapability.” For those of you familiar with the concept of “capacity” in medicine, this is basically just the legal term that NC uses to talk about patients who lack capacity16. The definitions section explains:
(4) "Incapable" means that, in the opinion of a physician or eligible psychologist, the person currently lacks sufficient understanding or capacity to make and communicate mental health treatment decisions.
If a person is judged to be incapable, they can be voluntarily admitted to a psychiatric facility either: (1) by their health care power of attorney (HCP) -or- (2) pursuant to a previously executed “advance instruction for mental health treatment.”17
If they are admitted by their HCP, the HCP is able to consent to voluntary admission and treatment on behalf of the patient.
If admitted under a previous advance instruction, they can only be held for 15 days before the facility either needs to release them or file for involuntary commitment.
Finally, if the person does not have an advance instruction or HCP -and- has been judged incapable -and- has not been judged incompetent (a different thing we’ll get to later):
the legally responsible person for the incapable adult shall be one of the persons listed in subdivisions (3) through (7) of subsection (c) of G.S. 90-21.13… provided that the persons… shall not have the authority to admit an incapable adult to a 24-hour facility18 where the adult will be subject to the same or similar restrictions on freedom of movement present in the State facilities for the mentally ill.
I think that the whole “freedom of movement” thing refers to locked units, but I can’t tell. So basically: no HCP or advance instruction, no voluntary admission.
Incompetent Adults
Yes, incompetency and incapability/incapacity are two distinct concepts in the law. Surely, this has never been a source of confusion.19
Incompetency is a legal determination made by a judge (or in NC, the county clerk) that an individual:
…lacks sufficient capacity to manage the adult's own affairs or to make or communicate important decisions concerning the adult's person, family, or property…
For these individuals, a court appoints a guardian. Full guardians have quite broad power, though the court may also determine that a limited guardianship20 is more appropriate.
Important for me is § 35A-1241(a)(3), which states that:
The guardian is able to give consent and approval for medical and psychological care
Unless their ward has already designated a HCP and the clerk did not cancel it when guardianship was awarded
Anyway, at the end of the day, admission for incompetent patients seems to follow the same general rules as those for incapable patients, except that (1) the facility needs notify the local district court that the patient has been hospitalized within 24h, (2) a hearing needs to be held within 10 days, wherein the court will determine whether or not the patient requires treatment for mental illness.
Discharge happens whenever the treating facility or the court determines that inpatient treatment is no longer necessary. The guardian can request discharge, but if the facility disagrees, they have to go back to court to request a reconsideration.
Patients with Developmental Disabilities
North Carolina — like MA — treats people with intellectual and developmental disabilities differently from people with mental illness.
I would really prefer not to have to get into definitions here, but I did this to myself. Chapter 122C defines a “developmental disability” as:
A severe, chronic disability of a person that satisfies all of the following:
a. Is attributable to a mental or physical impairment or combination of mental and physical impairments.
b. Is manifested before the person attains age 22, unless the disability is caused by a traumatic brain injury, in which case the disability may be manifested after attaining age 22.
c. Is likely to continue indefinitely.
d. Results in substantial functional limitations in three or more of the following areas of major life activity: self-care, receptive and expressive language, capacity for independent living, learning, mobility, self-direction, and economic self-sufficiency.
e. Reflects the person's need for a combination and sequence of special interdisciplinary, or generic care, treatment, or other services that are of a lifelong or extended duration and are individually planned and coordinated; or when applied to children from birth through age four, may be evidenced as a developmental delay.
And an “intellectual disability” as:
A developmental disability characterized by significantly subaverage general intellectual functioning existing concurrently with deficits in adaptive behavior and manifested before age 22.
Overall, I think these definitions are fine21, but Chapter 122C has special rules for individuals with developmental disabilities. First, it only seems to allow for admissions to “[facilities] for individuals with intellectual or other developmental disabilities.” How do you know that a facility is specifically for those types of individuals? Can they be for both mentally ill and intellectually disabled patients? I found some stuff in the NC Administrative Code (10A NCAC 26C .0101), but it didn’t clear things up very much other than making it clear that there are certain designations that can be applied for.
This also raises the question of where individuals with autism are considered to fit within the North Carolina schema. Autism (in some cases) can pretty clearly meet the definition of “developmental disability” above. It also can meet the definition of “mental illness” and is a formal psychiatric diagnosis in the DSM to boot.
There’s some other unique rules about admissions and discharges, but I’m just going to ignore those for now and hope that I don’t regret the decision later.
The biggest unanswered question I am left with after all of this is whether or not there are special restrictions around particular medications or treatments for patients who are incapacitated or ruled incompetent. In MA there is a special type of guardianship (a Rogers Guardianship) that must be awarded for a guardian to consent to antipsychotic drugs on behalf of their ward. No Rogers, no antipsychotics. I don’t see anything like that in the NC laws or on a (very) cursory search of the case law.
Next time we’ll go through the involuntary commitment part of 122C, including definitions of what things like “danger to self or others” mean. You know, the most interesting stuff that I thought I would be writing about until I took this detour through the voluntary sections.
Thanks, as always, for reading!
Pro Tip: Whenever someone says that their understanding of a complex subject can be summed up in a meme, it’s usually an indication that they do not have a complete understanding of that subject.
Can you guess where I think I’m going to end up post-residency?
In other contexts known by the term “kidnapping”
Don’t come at me with “well technically it’s the judge, blah, blah.” You and I both know that (1) An initial 72h hold in most places is stupidly easy to obtain and usually just requires our say-so. (2) That we’re the ones who are really driving the car when it comes to civil commitment hearings. In what percent of your commitment hearings do you feel like your patient was adequately and fully represented? For me it’s been less than 10%.
“Case law, also used interchangeably with common law, refers to the collection of precedents and authority set by previous judicial decisions on a particular issue or topic.”
i.e. Diseases traditionally treated and managed by neurologists
The Diagnostic and Statistical Manual of Mental Disorders - aka what psychiatrists (kinda) use to diagnose people.
For those of you who don’t know. The DSM-5 was supposed to eliminate almost all of the traditional personality disorders (except borderline and one other, I think?) and replace them with a spectrum model based off of the much more empirical Five Factor Model of Personality. This was actually pretty close to happening until a bunch of rank-and-file psychiatrists got upset that things like Narcissistic Personality Disorder were being eliminated, and a letter writing campaign — led by John Gunderson (the father of the modern conception of Borderline Personality Disorder) — put enough pressure on the APA Board of Trustees to nix the whole thing. Yes, I am a bit bitter about it.
Yes, wow, very deep Dr. Wendel
A psychiatrist, psychologist, nurse practitioner, LCISW, or police officer
The technical term for this is “lying”
I’m not going to point out every ambiguity going forward — I would probably stop writing and you would definitely stop reading — but just keep in mind that the law is littered with these sorts of uncertainties.
In other words, it would be fine if they produced a copy of a physical exam done by their PCP 10 days ago.
Yes, things like this last one are actually things that inpatient units will say.
For those interested, capacity inquiries have been heavily shaped by the “Appelbaum Criteria” (paper here) which requires that the patient demonstrate: understanding of the relevant information; appreciation of the risks/benefits of the proposed intervention and its alternatives; the ability to give a rational and more-than-superficial explanation of their decision; the ability to indicate a clear choice, consistently.
What you might know as an “advance directive”
A 24-hour facility is a statutory term for: “a facility that provides a structured living environment and services for a period of 24 consecutive hours or more and includes hospitals that are facilities under this Chapter.”
If you ever need to keep a Consult/Liaison psychiatrist busy, just ask them innocently what the problem is with asking them to evaluate patients for “competency to make medical decisions.”
Where, for example, the guardian controls a person’s finances, but not other aspects of their life.
There’s some weird stuff here in that “intellectual disability” requires meeting the criteria for “developmental disability” but I don’t think this really matters.




As a med student I don't think I'll go into psych because there's no evidence for involuntary commitment for suicidality, and I'd be expected to section people all the time... I'm huge on human rights, and need a compelling reason to take someone's freedom away from them, (like severe manic psychosis), and also am an advocate for making suicide more accessible for competent adults (I want it as an alternative to a nursing home when I get old!)... Another unpopular opinion in psych circles.
There was a case brought against an ER physician for not involuntarily admitting a man who committed suicide 18 days after an ER visit.
Patient at time of visit was passively suicidal; but nothing you’d involuntarily cert over. After patient’s wife left him; and he commit suicide; patient’s wife then sued the doctor.
So yes the statute might protect you from NOT hospitalizing someone; but you are still very very liable to being sued. With the attendant financial and emotional stress…