Stop Twisting Yourself Into Knots About QTc
Some Points about QTc and Psychopharm in Psychiatry
When you start residency, you’re taught some things that you absolutely must pay attention to or it will be very bad and people will die and you wouldn’t want that to happen would you? I seem to have some sort of disorder that makes me ask questions like “Well, what does ‘very bad’ mean… like, in numbers?” When the answer is “…uh, like, pretty high, probably?” a bizarre form of synesthesia afflicts me as the words “colace” and “essential medicine” flash before my eyes, and then I wake from a fugue state and discover I’ve written a whole essay1.
QTc prolongation happens to be one of those very bad things. It results in recommendations in psychiatry consult notes like “obtain daily ECGs2, hold all antipsychotics for QTc >500, trend magnesium, potassium, and replete as necessary” whenever a patient is put on an antidopaminergic3 to avoid the risk of ~Torsade de Pointes~4 (aka TdP).
This seems pretty trivial, but it can matter quite a bit. Sometimes it means that patients get taken off of antipsychotics that have kept their psychosis at bay for decades, or that have kept a delirious patient from extubating themselves. It also results in unnecessary medical costs. My hospital bills (an insane!) $2435 for an ECG, $133 for a metabolic panel that includes potassium, and $78 for a magnesium level. You can see how quick the costs add up here.
Oh no it’s Cardiology Time… Again
That’s QT
QTc stands for “corrected QT-interval.” The QT-interval is the period of time from the start of the Q-wave, which represents depolarization of the intraventricular septum, to the end of the T wave, which represents repolarization of the ventricles. You can see a visual representation of this on the ECG below.

Because the QT interval naturally changes with heart rate (HR), the QTc was created as a way to standardize the QT-interval to allow for comparisons across heart rates. The QTc estimates what the QT-interval would be in a particular individual at a HR of 60 beats per minute (BPM).
For reference, the normal QTc ranges are (roughly):
Males: 350-450ms
Females: 360-460ms
The first of these correction formulas is called the Bazett formula, which uses the RR-interval, which is the just the distance between the peak of the R-waves:
This formula was published in 1920 using a very small (n=39!) number of young, mostly 18-19 year-old, subjects. The paper is a fascinating read, primarily because it seems to be at a transition point from mechanical methods6 to electrical methods of observing the action of the heart; it’s worth remembering that this stuff used to be really hard and now you can just get an ECG in 2-3 minutes without a cardiologist in sight.
In the same year, Louis Sigurd Fridericia published his paper7 with his own QTc equation, which was based on 50 healthy volunteers, 28 males and 32 females, from ages 3-81.
Bazett’s was apparently more popular due to ease of calculation, though it was understood that it lost accuracy in patients with particularly fast or slow heart rates (i.e. not between 60-100bpm).
Despite this, it somehow took 63 years until Hodges developed a linear formula8. I would include the details but the paper appears to have been scoured from the face of the Earth, so, sorry:
In 1991, the authors of the Framingham Heart Study, presumably after realizing that pocket calculators had been cheap and affordable since the 80s, thought that maybe “this one is easier to calculate” was not the best reason to still be using Bazett’s formula, and also maybe that the default equation for QTc shouldn’t be based on a study of a few dozen teenagers in the 1920s, so how about 5,018 men and women from the ages of 29-62 instead? Thus the Framingham formula was born:
Rautaharju, not to be outdone, developed a New Age Criteria, sorry, New age- and sex-specific criteria after analyzing the ECGs of 57,595 individuals, in a move that I can only hope kicks off a series of increasingly large studies that result in cardiologists single handedly fixing the first-world’s replacement birth-rate problems in search of additional study participants. And lo! Unto cardiology a new formula was born:
Please Stop Using Bazett’s
There have been many studies that have compared the utility of each of these equations. Every one I can find indicates that we should pretty much stop using Bazett’s:
Optimal rate correction was observed using Fridericia and Framingham; Bazett performed worst… Fridericia and Framingham correction formulae showed the best rate correction and significantly improved prediction of 30‐day and 1‐year mortality. With current clinical standards, Bazett overestimated the number of patients with potential dangerous QTc prolongation, which could lead to unnecessary safety measurements as withholding the patient of first‐choice medication.
The Fridericia correction, but not the Bazett correction, was independent from heart rate and allowed adequate QT correction
The distributions of QTc based on Fridericia, Framingham, and Hodges formulae were similar but Bazett's was significantly wider. Whether for males and/or females, the middle range of HR from 60 to 99 bpm has similar upper normal limits of QTc for all formulae except Bazett. Numerous references recommend 420 to 440 ms as the threshold for reporting prolonged QTc when using Bazett's formula. Based on this database, 30% of apparently normal ECGs would be reported as having abnormal QT intervals for the 440 ms threshold, or 10% if 460 ms is chosen, compared to <2% for the other formulae.
You get the point.
Mystifyingly, Bazett’s continues to be the default equation used by the vast majority of digital ECG machines, at least in my hospital. As you may have guessed from the quotes above, this results in a lot of over-estimated QTc values, which results in people panicking and consults to psychiatry about what alternative medications should be used for agitated patients.
I have no idea why this is the case. Are the ECG machines that hard to reprogram? Are hospital administrators colluding with the Bazett Estate and hiding the keys? I can think of no other reason as to why cardiologists haven’t risen up in revolt against Big Bazett and stormed the tech closets of the medical floors around the country.
QTc and Cardiac Risk
Of course, the whole point of measuring the QTc is to predict how at-risk a patient is for developing TdP and other life-threatening ventricular arrhythmias, so let’s talk about that.
Drew et al. a 2010 paper on preventing TdP in hospital settings notes that:
each 10-ms increase in QTc contributes approximately a 5% to 7% exponential increase in risk for TdP in patients with prolonged QTc. Therefore, a patient with a QTc of 540 ms has a 63% to 97% higher risk of developing TdP than a patient with a QTc of 440 ms. Data from congenital LQTS [Long QT-Syndrome] studies indicate that a QTc >500 ms is associated with a 2- to 3-fold higher risk for TdP. Likewise, case reports and small series of patients with drug-induced TdP show similar increased risk when the threshold of QTc >500 ms is exceeded.
Sounds very spooky! But we all know the quote about “lies, damned lies, and statistics,”9 so let’s look at what the actual numbers are.
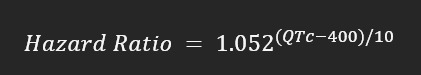
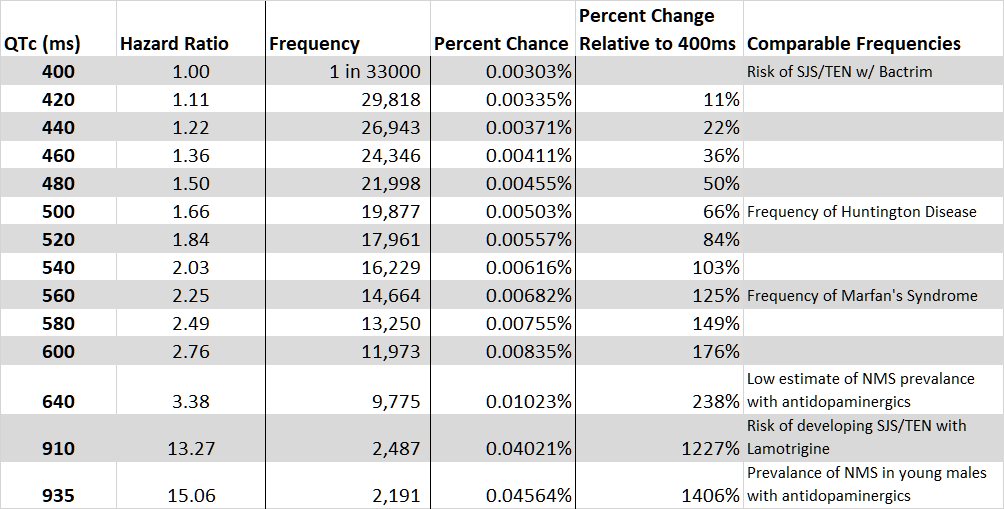
Drew et al. reference Moss et al. 1991 whose findings are later refined in Moss et al. 1993. This 1993 paper provides an equation for a hazard ratio10:
This equation tells you about an individual with LQTS’s risk of “arrhythmic syncope11 or probable long QT syndrome-related death” — over any period of time — relative to someone with a QTc of 400ms. Since we are going to be focused on drug-induced QTc prolongation it is worth including this Moss et al. comment:
It is likely that this hazard ratio per unit increase in QTc, derived from the long QT syndrome population, is of a similar order of magnitude for drug-induced QTc prolongation.12
Of course, you need to know what that baseline risk is for this number to mean anything. Beach et al., 2018 puts the base rate for these events somewhere between 1 in 16,000 to 1 in 50,000 — a staggeringly large range — but we’ll have to make due.
Above is a table that shows the change in frequency for the upper, lower, and mean points in that range. If these numbers feel useless and untethered from reality, that’s because they are. How frequent is 1 in 30,117 really? I’m going to simplify this a bit in the next few tables by just using the mean of the range.
Hopefully this should help to put things into perspective a bit more.
At a baseline of 400ms, the risk of someone spontaneously developing a life-threatening ventricular arrhythmia is about as common as developing SJS/TEN (a severe immune reaction that has a similar mortality rate to TdP) while taking the antibiotic Bactrim. A 1 in 33,000 chance. This website informs me that Bactrim accounted for 6.5% of the 211.1 million antibiotic prescriptions written in the US in 2022, which is ~13.7 million scripts; in my personal experience I have never met a physician who was shy about prescribing Bactrim because of the risk of SJS/TEN outside of patients with a history of the same.
The Drew et al. paper above is technically correct that the patient with a QTc of 540ms has almost a 100% higher risk of developing TdP than a patient at 440ms. They are also correct that the risk curve here is exponential. What they seem to be missing is that these probabilities are so small that they are basically not worth paying attention to.
Indeed, the reason why I suddenly had this table jump to 910ms13 was to prove this point! Lamotrigine, an antiepileptic and mood stabilizer, also carries a risk of SJS/TEN of about 0.04% or 1 in 2500 individuals14. In medical school and residency, this fact is drilled into our heads and when we prescribe it we make sure to minimize this risk by going up slowly on the dosage and warning our patients to stop taking it if they develop a rash.
Does this deter us from prescribing it in the first place? Not really. This website says that in 2020 about 1.7 million patients were on lamotrigine. For comparison, here are estimations of the number of patients on some other medications in 2020:
Sertraline: ~7.8 million
Bactrim: ~3.5 million
Valproate: 910k
What gives? Why are we freaking out about QTc in the 500s — or even into the low 600s — when we are clearly plenty happy to prescribe a medication like lamotrigine that carries a 5-8x higher risk of a similarly deadly side-effect?
A few ideas:
First, training is long and complicated, and there are a dozen different rules very similar to “stop QTc prolonging drugs past 500ms” that we are taught at various points in our training. Generally, we assume that the people teaching us these rules know what they’re talking about, and that part of our job as trainees is to be mindful about our relative lack of experience and not go loading up people with IV haloperidol just to make sure that their attending was actually correct about the QTc thing. Nobody has enough time to go verify each and every one of these rules, and I’m pretty sympathetic to this.
Second, I think humans are pretty statistically illiterate and this is just another example of that. I find this less forgivable, especially for groups of very smart people like Drew et al. whose entire job is to lay out the facts in a legible fashion that do not overstate or understate the evidence. Providing readers with comparisons to similarly frequent/risky events when discussing risk should be a core part of how we communicate statistics!
Third, is that the academic and public incentives are generally aligned against writing papers titled “Why You Shouldn’t Care So Much About Prevention of Torsade de Pointes in a Hospital Setting,” in which the conclusion is “We recommend that y’all chill out a little bit, this QTc stuff isn’t a big deal in the grand-scheme of things.” It’s just not aligned with this idea that physicians are supposed to be discovering ways to do things to save more lives.
My final, and most steel-man-y idea is that everyone has already thought out this problem, has the appropriate statistical context, and decided that actually a 1 in 20,000 chance is too high. The discrepancy with lamotrigine prescribing indicates that we should be prescribing far less lamotrigine, not that we should be more comfortable with higher QTc’s! I know that this mindset exists — I see something similar in the idea that doctors should act exclusively in the best interests of whatever patient they are seeing at the moment — but I just can’t agree. Risks exist everywhere, whether we like it or not, and trying to drive it down as low as possible will result in sub-optimal care that will result in worse outcomes that are only technically not our fault.
Oops, sorry, there’s a little more I found when editing this/What About QTc Measurement Variability?
Looking at such small numbers made me wonder how much normal variability you’d see in the QTc’s of healthy individuals. Measurement error is always a thing, and at the end of the day we’re just sticking electrodes on someone’s skin.
Turns out that other people wondered about this too. Hnatkova and Malik wrote a whole paper that pointed out things like:
Gueta et al. did a study that found that the mean change in QTc between ECGs in healthy individuals over a mean period of 1 year was 23ms.
Lead II is assumed to contain the longest QT interval, and so it’s typically used to measure the QT-interval for correction. However, an analysis of 8,000 ECGs showed that Lead II only contained the longest QT interval 10% of the time, and was off by up to 50ms in some cases
The thickness of the average line on a modern ECG tracing is about 0.5mm, which corresponds to about 20ms, which makes manual correction very susceptible to individual variability. The authors say that this is mostly solved by modern machine computation which isn’t susceptible to this problem.
Changes in HR do not result in instantaneous changes in QTc, instead the QTc responds over the course of minutes. This is called heart rate hysteresis. Unfortunately, machine estimates only use 10-second averages of HR. In one example they give, they look at two ECGs in a healthy individual separated by only 20 seconds, but with two very different machine estimated heart-rates; 73 and 53 BPM. The 10-second estimation produced QTc’s of 411ms and 458ms, a difference of 47ms. When a 5-minute history of HR was used, the QTc’s were 417ms and 419ms, a difference of only 2ms!
They conclude that:
…[Experiments] still suggest that with heart rate changes in excess of 15 or possibly 20 beats per minute, no fixed correction formula can be relied on for the purposes of clinical decisions…
And ultimately:
The QTc variability seen in clinical practice can (and should) thus be substantially reduced if paying attention to measurement and interpretation details… If using a drug with a known proarrhythmic potential combined with expected large heart rate effects, patient‐specific QT/heart rate profile should first be established so that subsequent safety monitoring can separate the drug adverse effects from the heart rate adaptation.
Yeah, uh, we don’t do that at all.
The Psychopharmacology of QTc Prolongation
My hope is that the argument I’ve just made is strong enough to convince you that we should, in fact, chill out about QTc prolongation. At the very least it should be clear that there is no good rationale for an absolute contraindication to QTc prolonging medications for patients with a QTc >500.
Maybe you’ve bought the whole argument, but you’re going to be consulting to teams that certainly won’t. Or maybe you’re willing to buy that last part about no absolute contraindications, but you’d still like to minimize risk where you can…
Fine, I’ll write the rest of the essay15.
Delayed Rectifier Potassium Channels and You
If you went to medical school or studied neurobiology in undergrad/grad school, you might recall how neuronal depolarization and repolarization works. Try to forget about all of that, it’ll make this next part easier.
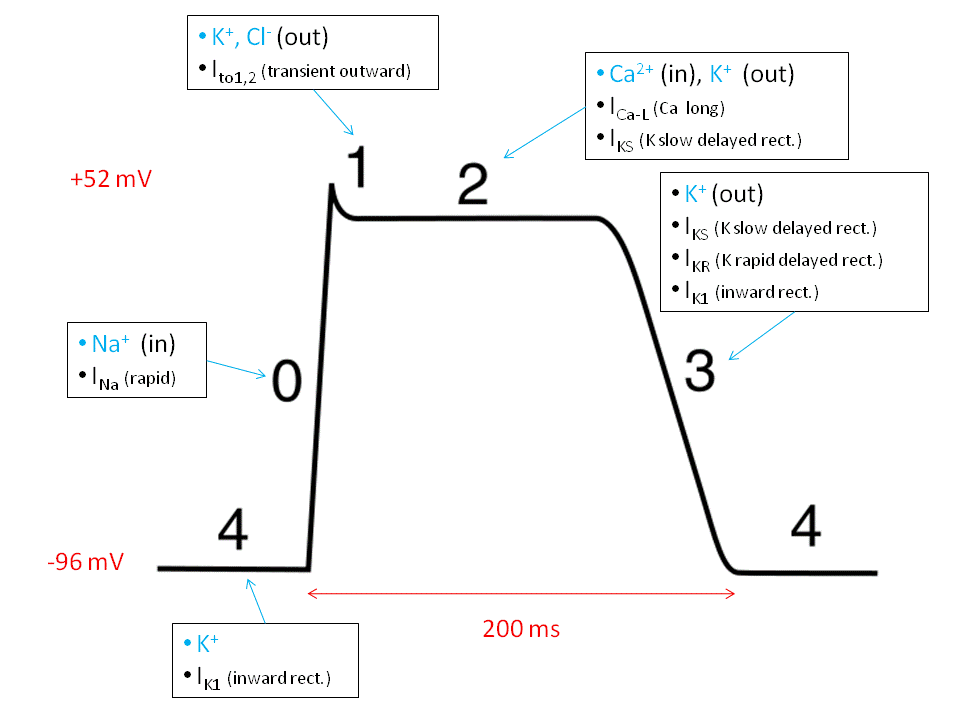
This is a cardiac action potential. Sodium flows into the myocyte to kick off the depolarization, and then things get weird. Following depolarization, potassium flows out of the cell, but it is counterbalanced by an influx of calcium ions, which results in a sustained depolarization that is the phase-2 plateau. Eventually, the calcium channels close, and a few different types of potassium channels open to push the membrane potential back down. At the end the cell is repolarized and ready to do the whole thing again.
Iκs and Iκr16 are delayed rectifier channels17. Blockade/malfunction prevents potassium flow across the membrane, lengthening the time that it takes for repolarization, thus resulting in QTc prolongation.
Mutations in Iκs and Iκr account for ~65% of the genetic forms of Long QT-Syndrome, but blockade of Iκr is the usual mechanism of drug-induced QTc prolongation due to binding of the hERG1819 subunit. As far as I know, all of the medications I talk about (certainly the antidopaminergics) below are thought to prolong the QTc via this mechanism.
The Drugs Themselves
There are a handful of medications in psychiatry that are known as “QTc prolonging” medications, though not necessarily because they actually prolong the QTc interval.
For example, I was taught in medical school that clozapine prolongs the QTc interval. It turns out that it just made people tachycardic, and because previous studies were using Big Bazett’s™ formula, their QTc was over-estimated.
Ziprasidone, citalopram, and IV haloperidol are also the cause of QTc-related hand-wringing, but how much do they actually prolong the QTc?
One sec.
Before I show you the answer, think about what you’ve read so far and ask yourself this question:
“How much would a drug need to increase the QTc, on average, for me to hesitate in prescribing it?”
Got a number?
Ok.
(Sorry, I have to stall for the desktop readers)

Keep in mind, these are all at therapeutic doses20. The numbers don’t change even if you look just at the high end of the dosing curve, I checked.
If your number was anywhere near these, I don’t believe you. Anyone with a risk tolerance that low would’ve looked at the title of this essay and thought, “Nah, I’m good, thanks” and then probably return to bubble-wrapping the patients that are just about to be discharged or re-consulting psychiatry for a 5th capacity eval on the demented lady who insists that her hip isn’t actually broken and she has somewhere she needs to be.
“But what about IV Haldol?”
So glad you asked!
Beach et al. 2020 does a nice review of the literature and cites multiple large RCTs (mostly in critically ill individuals) that show no differences in QTc relative to placebo. They also include this gem of a quote that is absolutely emblematic of medical mythology:
It is worth noting that a commonly cited source for the claim that [IV haloperidol] prolongs the QT interval is an unpublished observational study from 1995 involving 6 patients that was never subject to peer review.21
I rest my case.
Takeaways
At the outset of this section, I want to be pretty clear about something. I realize that what I am about to say is pretty bold for someone who hasn’t completed their residency. As I was writing this essay, I thought this section was going to have some collection of measured conclusions with reasonable caveats, not a single, definitive claim. I’ve tried to mitigate my knowledge gaps by passing a draft of this around to multiple people with more experience than me, and I asked around to see if there was a cardiologist willing to read this over before publication.
Even with all of that, my instinct was to hedge my conclusions — even when I didn’t think it was justified — both to assuage my own discomfort with making a bold claim, and in the hope that it would make you, the reader, more likely to trust me. As much as I want to do that, it would feel dishonest.
Much of what underlies the illness I have that causes me to ask questions like the one at the beginning of this essay, is a feeling that it is important to try and discover which parts of our medical practice exist primarily to help make ourselves feel less anxious/better about our decisions, and which exist because they improve the lives of our patients and the system that we are all beholden to. Part of why I like to teach is because it drives me to ask these questions. Part of why I write is because I think that those answers, and how I get to them, are worth sharing with you. Medicine and its practitioners cannot worship at the altar of the Scientific Method only to refuse where it leads when the evidence leads us to bold and uncomfortable conclusions. It would be a failure of me as a teacher to advocate for this unflinching view, only to shy away from it at the last moment, here.
With that lengthy (overwrought? probably.) preamble out of the way…
The measurement errors pointed out by Hnatkova and Malik are a major problem. It seems like almost no studies actually correct for heart rate hysteresis — Hnatkova and Malik specifically mention that the Gueta et al. paper did not — which calls into question the QTc measurements underlying most of this data. Certainly we do not regularly correct for this in the clinical settings I work in.
I’m assuming that the hysteresis problem doesn’t make all of that data completely garbage, because we still diagnose LQTS with ECGs and we know that there is an underlying ion channel pathology in these individuals that produces those changes.
Even assuming that the hysteresis problem didn’t exist, we’re still stuck with having to confront the fact that drug-induced QTc changes induced by our psychotropics are so small that they are statistically irrelevant. This seems to be the case even in the critically ill (see: IV haloperidol), and in individuals with LQTS; recall that the hazard ratio equation used above is based off of risk in patients with LQTS.
As I said, the conclusion is straightforward:
For the vast majority of patients, the risks of QTc prolongation with extant psychotropic medications is not clinically relevant, and there is no virtually no clinical utility in its consideration when selecting a treatment agent. Outside of idiosyncratic cases22, it would be well within the norm of how we deal with risks of similar magnitude to do nothing more than be aware of its existence, as we do for SJS/TEN with Bactrim and NMS with antidopaminergics.
P.S. I’ve made available the spreadsheet that I used to create the tables in this essay here on Google Sheets. It’s formatted to be printable onto a single sheet of paper as a teaching tool, please feel free to use and edit this as long as you give me credit for its creation.
P.P.S. A thank you to Dr. Christian Smith, Dr. Dallas Hamlin, and Dr. Dan Augustadt for their review and advice on the drafts of this article.
What follows below is the essay, btw.
Electrocardiogram aka an EKG.
I use the term antidopaminergic instead of antipsychotic.
‘Torsade de Pointes’ translates to “twisting of the points” and is the result of disordered electrical activity in the heart that produces a characteristic ECG pattern. The sources I’ve seen estimate that TdP results in cardiac death in up to 10% of patients, though about 50% are asymptomatic!
$215 of this is a hospital fee, $28 is a physician fee. My insurance would cover $112, so I would still be on the hook for $122.
Using stethoscopes, blood pressure, touch, and literally looking at the chest and visible vasculature.
The original is in German, sorry.
I am totally unable to find the original text for this, though I frequently find a citation that leads nowhere: Hodges MS, Salerno D, Erlinen D. Bazett's QT correction reviewed: evidence that a linear QT correction for heart rate is better. J Am Coll Cardiol. 1983;1:694
A version of which is attributed to the French physician François Magendie (of foramen fame), who was arguing against bloodletting by saying “Thus the alteration of the truth which is already manifesting itself in the progressive form of lying and perjury, offers us, in the superlative, the statistics.”
Additional risk beyond a similar “normal” individual. For example, a hazard ratio of 2 means that an individual is twice as likely to experience the harmful event than the control.
I’m guessing that this is similarly severe as “death.”
This quote warrants its own set of caveats, namely that there are those that take issue with the idea of this equation being accurate for all causes.
To be honest, I’m not really sure that a QTc this long is compatible with life. Googling for “longest recorded QTc” didn’t get me anywhere. That’s a bit besides the point though, it’s about illustrating how far away these comparison risks are.
This is assuming the (now) standard slow up-titration in dosage. Previously the risk was 1 in 100(!) when jumping straight to clinically effective doses.
But only because I had most of it written before I wrote that joke. Seriously, I don’t think you really need the rest of this essay.
The ‘s’ is for slow and the ‘r’ is for rapid. Confusingly, Iκs channels actually open earlier than Iκr channels, but the Iκur (ultra-rapid) channels open before Iκs.
‘Delayed’ because they open after the potassium channels that are open in phase-1. ‘Rectifier’ because they ‘rectify’ the membrane voltage back towards its resting potential.
human Ether-à-go-go-Related Gene (hERG) so named because, “when [fruit] flies with mutations in the Ether-à-go-go gene are anaesthetized with ether, their legs start to shake, like the dancing at the then popular Whisky a Go Go nightclub in West Hollywood, California.”
Is genetic nomenclature just a series of obscure jokes about fruit-flies? Yes, yes it is.
“hERG” is also the sound I imagine someone making when they have a heart attack, which I think is at least a little funny.
Also remember, the median variability in healthy individuals was 23ms!
All 6 of these were critically ill and some getting more than a GRAM of haloperidol a DAY.
e.g. a patient who develops TdP every time they’re put on a combination of a macrolide and haloperidol.






Excellent, this post has done wonders for me as a pharmacist who kind of refuses to freak out over stacking just a few QTc prolongers but was secretly worried he was stupid for seemingly being the only one.
Next level, this is what becoming a physician is about, getting to this level of understanding
Thank you